Artificial Intelligence (AI) and Machine Learning (ML) are driving a profound transformation in medicine, reshaping diagnostics, patient management, and the very framework of care delivery. Leveraging AI-ML for healthcare enables clinicians to extract actionable insights from massive datasets, improve diagnostic accuracy, and personalize treatment—ushering in an era of precision health. This article examines the evolution, key applications, future directions, and challenges of AI/ML in healthcare in 2025.
The Foundations: What Are AI and Machine Learning in Healthcare?
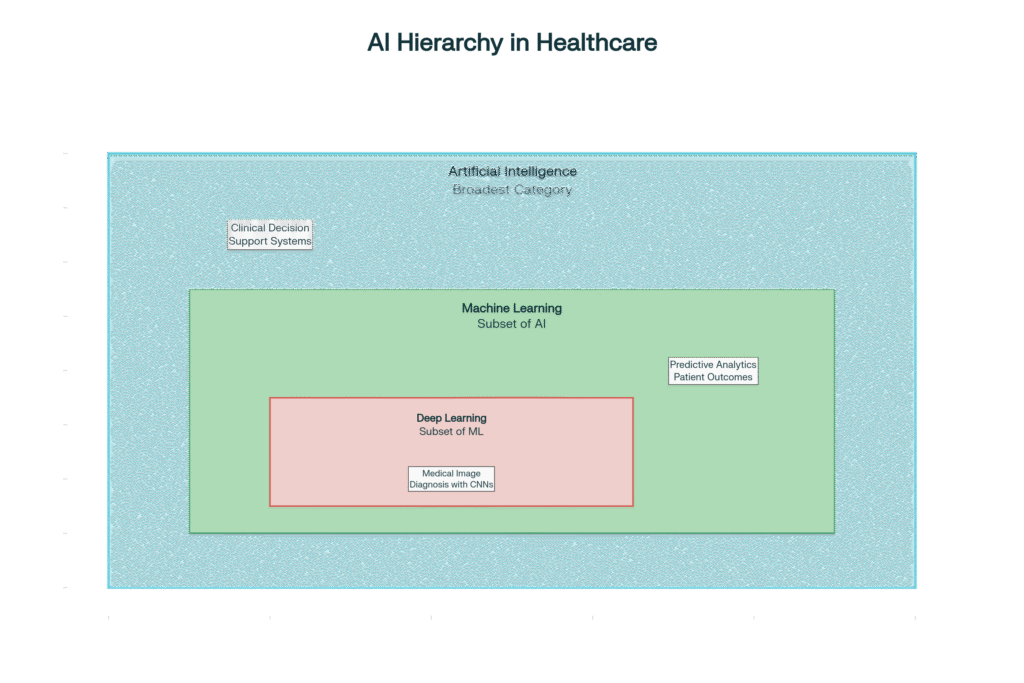
AI encompasses computer systems that mimic human intelligence, including reasoning, learning, and problem-solving, while ML is a subset of AI where machines learn patterns from data without explicit programming.
- Machine learning algorithms process clinical data—such as lab results, imaging, physician notes, and wearable stats—and learn to recognize complex patterns that inform faster and more accurate decision-making.
- Deep learning, a specialized ML form, uses artificial neural networks to perform advanced tasks like image analysis, language processing, and even robotic surgery.
Key Applications: How AI/ML Are Disrupting Healthcare
1. Diagnostics and Disease Detection
AI systems now assist in screening and early detection of diseases across specialties.
- In oncology, AI-driven imaging analysis can spot cancerous lesions or tumors far earlier and more accurately than traditional techniques, improving patient survival rates.
- In radiology, convolutional neural networks (CNNs) interpret X-rays, CT, and MRI scans with high precision, detecting issues like fractures or brain tumors and reducing diagnostic errors.
- AI tools are also revolutionizing dental health, dermatology, and ophthalmology by identifying subtle abnormalities—sometimes missed by human eyes.

2. Personalized Treatment and Precision Medicine
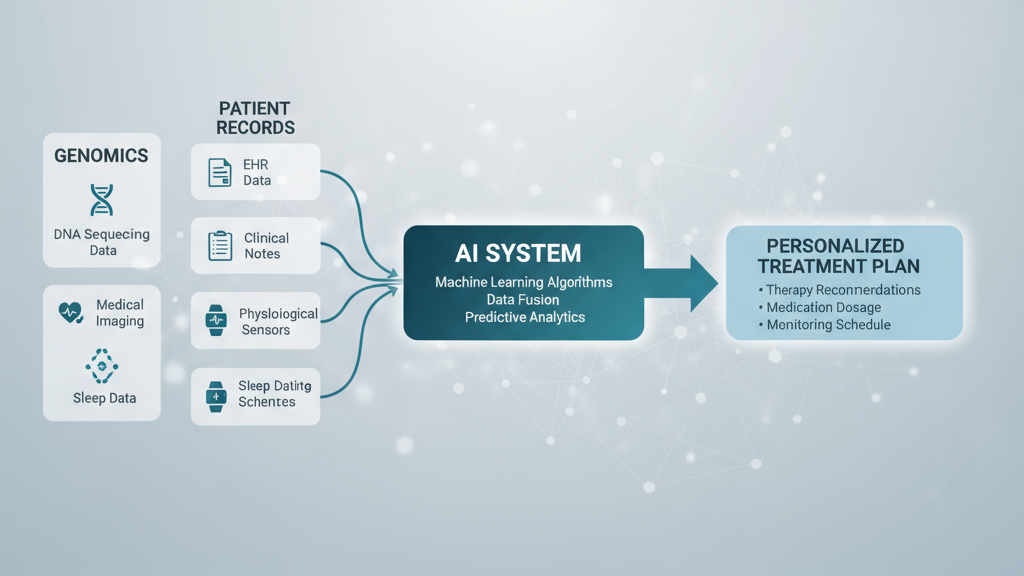
AI models analyze genetic, clinical, and lifestyle data to recommend customized interventions.
- ML algorithms select optimal therapies for cancer patients based on tumor genetics, improving outcomes.
- In cardiology, AI predicts the risk of heart events and guides medication or device choices.
- Personalized medicine becomes reality as AI tailors health plans to individual needs, even considering subtle data from wearables or home monitoring devices.
3. Drug Discovery and Development
AI accelerates the drug pipeline, identifying promising compounds, predicting protein structures, and optimizing clinical trials.
- For example, DeepMind’s AlphaFold uses AI to reliably predict protein folding, a breakthrough that enables faster, more targeted therapeutic development.
- By simulating virtual drug trials and screening molecular databases, AI slashes years—or even decades—from the process of bringing new medicines to market.
4. Virtual Health Assistants and Remote Monitoring
AI-powered chatbots and virtual assistants offer 24/7 patient support—answering questions, triaging symptoms, and guiding medication adherence.
- Smartwatches and IoT-enabled medical devices (“Internet of Medical Things”—IoMT) feed real-time health data to AI systems that alert clinicians to early risk signals.
- During pandemics and in rural areas, telehealth platforms use AI to triage and monitor patients remotely, enhancing access to care.

5. Optimizing Healthcare Operations
AI supports administrative efficiency, automating scheduling, billing, and electronic health records (EHRs), freeing up clinicians’ time.
- Predictive analytics enable better resource allocation (e.g., ICU beds, staffing), forecasting seasonal surges, and improving patient flow.
- AI-driven pattern recognition in EHRs also flags at-risk patients for follow-up or intervention.
How Does Machine Learning Work in Healthcare?
ML algorithms “learn” from data to predict, classify, or recognize patterns:
- Supervised learning: The system is trained with labeled data (e.g., known cases and outcomes) and learns to predict new outcomes.
- Unsupervised learning: The algorithm discovers patterns and relationships in large datasets without human guidance—useful in genomics and predicting new disease subtypes.
- Reinforcement learning: The AI “tries out” different strategies (such as treatment protocols in simulations), improving performance based on feedback.
These approaches power applications from risk prediction (e.g., sepsis, stroke) to the analysis of genomic data, and medical image classification.
The Future: Where AI and Machine Learning Are Heading
By 2030, experts predict even deeper integration of AI-ML into all healthcare domains:
- Ambient intelligence: Sensors and AI work in the background, continuously assessing patient health and environmental factors, intervening automatically if danger arises.
- Synthetic biology and immunomics: AI models will soon drive the custom design of therapies based on an individual’s immune response and genetic signature, promising breakthroughs for cancer, rare diseases, and neurological disorders.
- Federated learning: Hospitals can collaborate on model training without sharing raw patient data—addressing privacy issues while leveraging big data for population health.
- Digital twins: AI constructs virtual models of individual patients, testing possible interventions and predicting outcomes before actual treatment.
Challenges and Considerations
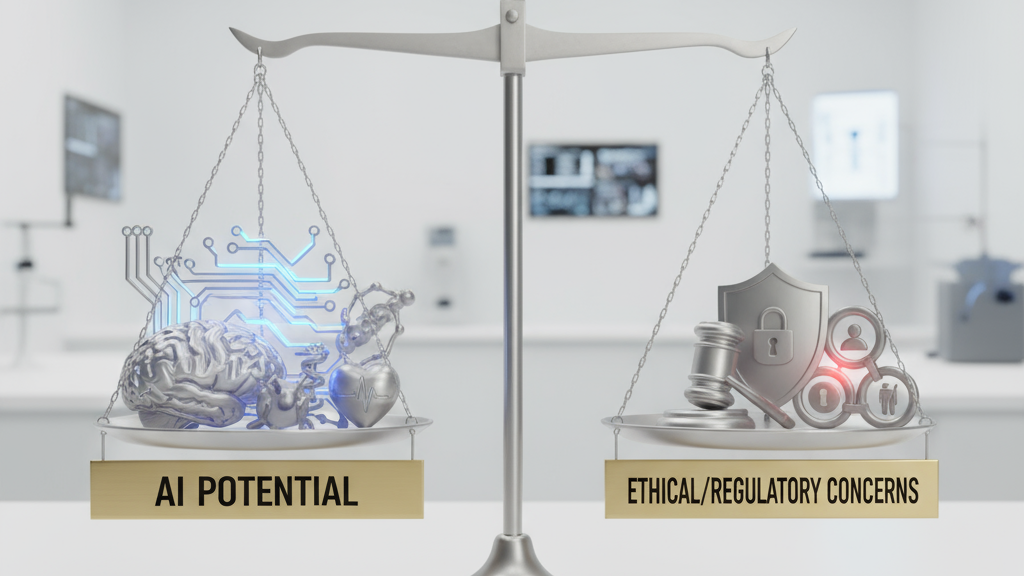
Despite remarkable promise, AI-ML in healthcare faces key challenges:
- Data privacy and security: Safeguarding sensitive patient information is a top concern.
- Algorithmic bias and fairness: If not properly managed, AI can perpetuate or amplify healthcare disparities due to biased training data.
- Transparency (“explainability”): Black-box algorithms make it hard for clinicians and regulators to understand how a decision was made.
- Clinical validation and regulation: Rigorous evaluation is needed to ensure AI solutions are accurate, safe, and effective—and that they complement, rather than replace, human expertise.
- Education and Integration: Training clinicians to work alongside AI systems and integrating new technologies into established workflows require institutional commitment.
Real-World Examples in 2025
Early Cancer Detection
AI algorithms in imaging systems are now standard in major oncology centers for early cancer detection, such as mammography for breast cancer and low-dose CT for lung nodules. These tools have reduced false negatives and improved survival rates by enabling intervention at the earliest stages.
Predictive Analytics for Chronic Disease
Major hospitals harness ML models to predict acute events in chronic illnesses (such as heart failure or diabetes) from remote monitoring data, allowing preemptive intervention and reducing costly hospitalizations.
Virtual Consultations and AI Triage
AI-driven chatbots offer triage advice and recommend when patients should seek in-person care, reducing pressure on emergency departments and improving care access—especially in rural and low-resource settings.
Personalized Drug Recommendations
Pharmacogenomic AI models analyze genetic profiles to predict medication efficacy and adverse effects before a prescription is written, improving medication safety and effectiveness.
Conclusion: The Road Ahead
Artificial intelligence and machine learning are undeniably reshaping medicine, bridging the gap between vast data and daily clinical decisions. AI already augments physician capabilities in diagnosis, patient engagement, and personalized care—delivering improvements in efficiency, safety, and outcomes. As ethical frameworks, validation standards, and clinician education evolve, the fusion of human expertise and intelligent machines promises a new era in healthcare—one defined by compassion, accuracy, and accessibility for all.

All facts, examples, and future trends cited in this post are supported by leading healthcare and AI authorities, including peer-reviewed journals and expert reviews.
Images described above should be generated to visually enhance key dimensions of the post and help readers better understand these complex, transformative technologies.
